Evaluation of an application based on artificial intelligence (AI) for the diagnosis of intestinal parasites and its potential use in Guatemala
DOI:
https://doi.org/10.36829/63CTS.v10i2.1344Keywords:
Intestinal parasites, Artificial Intelligence, accuracy, validity, digital microscopy, Convolutional Neural Network.Abstract
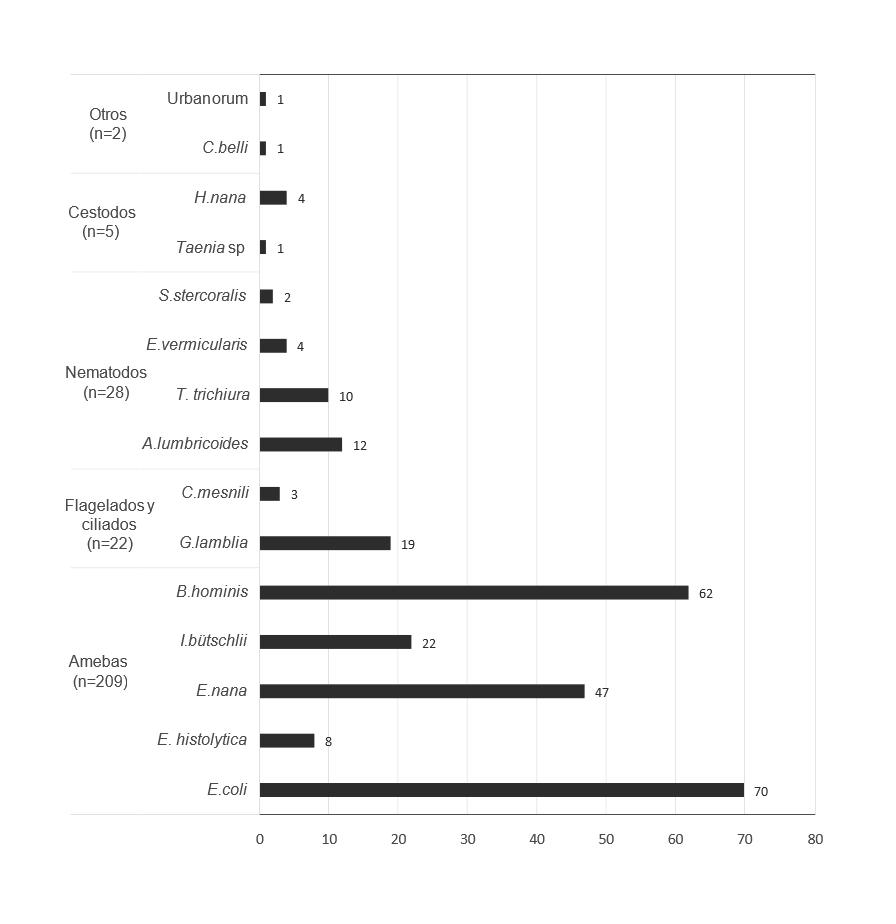
In Guatemala, intestinal parasitic infections represent one of the highest prevalence in Latin America; however, the observation of the microscopic morphology of these microorganisms continues to be the gold standard for their diagnosis. This methodology compromises the results in terms of the quality and availability of qualified personnel, subsequently the search for alternatives based on artificial intelligence (AI) represents a precise and complementary method in this field. The objective of this study was to determine the accuracy and precision of a free-to-use AI-based parasite identification tool. 314 samples were processed, 266 parasites were found, and 1,051 photographs were generated. From this file, 181 images were selected, as a reference standard, which was then compared with the identification through the AI application Parasite ID (https://parasite.id/). The analysis was carried out through the metrics of sensitivity, specificity, accuracy, agreement grade, and ROC curve, with a 95% confidence interval. The results for Parasite ID were sensitivity 25.2%, CI 95% [17.2,34.8]; specificity 79.5%, 95% CI [68.8,87.8]; accuracy 48.6%, 95% CI [41.1,56.1] and agreement grade 4.3%, 95% CI [-6.9,15.5]. The area under the ROC curve was 59.9%, 95% CI [52.4 – 67.1]. These results highlighted the need to improve the evaluated metrics and expand the catalog of parasites of clinical importance in the event that an application is developed at the local level.
Downloads
References
Abraira, V. (2001). El índice kappa. Semergen-Medicina de Familia, 25(5), 247-249.
Akoglu, H. (2022). User’s guide to sample size estimation in diagnostic accuracy studies. Turkish Journal of Emergency Medicine, 22(4), 177-185. https://doi.org/10.4103/2452-2473.357348
Arias, M. M., & Molina, M. (2013a). Características de las pruebas diagnósticas. Pediatría Atención Primaria, 15(58), 169-173. https://doi.org/10.4321/S1139-76322013000200013
Arias, M. M., & Molina, M. (2013b). El significado de los intervalos de confianza. Pediatría Atención Primaria, 15(57), 91-94. https://doi.org/10.4321/S1139-76322013000100016
Bogoch, I. I., Andrews, J. R., Speich, B., Utzinger, J., Ame, S. M., Ali, S. M., & Keiser, J. (2013). Short report: Mobile phone microscopy for the diagnosis of soil-transmitted helminth infections: A proof-of-concept study. American Journal of Tropical Medicine and Hygiene, 88(4), 626-629. https://doi.org/10.4269/ajtmh.12-0742
Bravo-Grau, S., & Cruz Q., J. P. (2015). Estudios de exactitud diagnóstica: Herramientas para su Interpretación. Revista Chilena de Radiología, 21(4), 158-164. https://doi.org/10.4067/S0717-93082015000400007
Cook, D. M., Swanson, R. C., Eggett, D. L., & Booth, G. M. (2009). A Retrospective Analysis of Prevalence of Gastrointestinal Parasites among School Children in the Palajunoj Valley of Guatemala. Journal of Health, Population, and Nutrition, 27(1), 31. https://doi.org/10.3329/JHPN.V27I1.3321
Donis, J. H. (2012). Evaluación de la validez y confiabilidad de una prueba diagnóstica (Assessment of the validity and reliability of a diagnostic test). Avances en Biomedicina, 1(2), 73-81.
Garcia, L. S. (2021). Practical guide to diagnostic parasitology (3rd ed.). ASM Press.
Gómez González, C., Pérez Castán, J. F., & Martin, J. L. R. (2007). Capítulo 8: Pruebas diagnósticas. Concordancia. SEMERGEN - Medicina de Familia, 33(10), 509-519. https://doi.org/10.1016/S1138-3593(07)73955-2
Landis, J. R., & Koch, G. G. (1977). The Measurement of Observer Agreement for Categorical Data. Biometrics, 33(1), 159-174. https://doi.org/10.2307/2529310
Mathison, B. A., Kohan, J. L., Walker, J. F., Smith, R. B., Ardon, O., & Couturier, M. R. (2020). Detection of intestinal protozoa in trichrome-Stained stool specimens by use of a deep convolutional neural Network. Journal of Clinical Microbiology, 58(6), Artículo e02053. https://doi.org/10.1128/JCM.02053-19
McHugh, M. L. (2012). Interrater reliability: The kappa statistic. Biochemia Medica, 22(3), 276-282. https://doi.org/10.11613/bm.2012.031
Metz, C. E. (2008). ROC analysis in medical imaging: A tutorial review of the literature. Radiological Physics and Technology, 1(1), 2-12. https://doi.org/10.1007/S12194-007-0002-1
O’Brien, S. F., & Yi, Q. L. (2016). How do I interpret a confidence interval? Transfusion, 56(7), 1680-1683. https://doi.org/10.1111/TRF.13635
OPS/OMS. (2022). Geohelmintiasis. https://www.paho.org/es/temas/geohelmintiasis
Parasite ID. (n.d.). Parasite ID | Home. Retrieved June 28, 2020, from https://parasite.id/
Quinn, J. A., Nakasi, R., Mugagga, P. K. B., Byanyima, P., Lubega, W., & Andama, A. (2016). Deep convolutional neural networks for microscopy-Based point of care diagnostics. arXiv:1608.02989, 1-12. http://arxiv.org/abs/1608.02989
Rajchgot, J., Coulibaly, J. T., Keiser, J., Utzinger, J., Lo, N. C., Mondry, M. K., Andrews, J. R., & Bogoch, I. I. (2017). Mobile-phone and handheld microscopy for neglected tropical diseases. PLoS Neglected Tropical Diseases, 11(7). https://doi.org/10.1371/JOURNAL.PNTD.0005550
Ryan, U., Paparini, A., Oskam, C. (2017). New technologies for detection of enteric parasites. Trends in Parasitology, 33(7), 532-546. https://doi.org/10.1016/j.pt.2017.03.005
Saboyá, M. I., Catalá, L., Nicholls, R. S., & Ault, S. K. (2013). Update on the Mapping of Prevalence and Intensity of Infection for Soil-Transmitted Helminth Infections in Latin America and the Caribbean: A Call for Action. PLoS Neglected Tropical Diseases, 7(9). https://doi.org/10.1371/JOURNAL.PNTD.0002419
Smith, K. P., Wang, H., Durant, T. J. S., Mathison, B. A., Sharp, S. E., Kirby, J. E., Long, S. W., & Rhoads, D. D. (2020). Applications of Artificial Intelligence in Clinical Microbiology Diagnostic Testing. Clinical Microbiology Newsletter, 42(8), 61-70. https://doi.org/10.1016/j.clinmicnews.2020.03.006
van Lieshout, L., & Roestenberg, M. (2015). Clinical consequences of new diagnostic tools for intestinal parasites. Clinical Microbiology and Infection, 21(6), 520-528. https://doi.org/10.1016/J.CMI.2015.03.015
World Health Organization. (2017). Integrating neglected tropical diseases into global health and development: Fourth WHO report on neglected tropical diseases. https://apps.who.int/iris/bitstream/handle/10665/255011/9789241565448-eng.pdf
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 Blanca E. Samayoa Herrera, Anneliese Moller Sundfeldt, Martin Gil Carrera, Mildred Alquijay Pacheco.

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
El autor que publique en esta revista acepta las siguientes condiciones:
- El autor otorga a la Dirección General de Investigación el derecho de editar, reproducir, publicar y difundir el manuscrito en forma impresa o electrónica en la revista Ciencia, Tecnología y Salud.
- La Direción General de Investigación otorgará a la obra una licencia Creative Commons Atribución-NoComercial-CompartirIgual 4.0 Internacional









